JULY 27, 2020

FILE PHOTO: A lab at Methodist Dallas Medical Center testing samples for coronavirus disease (COVID-19) in Dallas. – Reuters/Cooper Neill
The United States might have more COVID-19 testing capacity than any other country. So why have we seen laboratories overwhelmed and many patients again waiting a week or more for results?
At the heart of the crisis is a reliance by public and private labs on automated testing equipment that locks them in to using proprietary chemical kits and other tools made by a handful of manufacturers.
The result: as infection rates spike nationwide, many labs aren’t running anywhere near capacity because of supply-chain bottlenecks, according to Reuters interviews with 16 hospital, state, commercial and academic labs and an analysis of state and city procurement plans.
A few companies – Cepheid, Hologic Inc, Roche and Abbott Laboratories – dominate this market. Their machines run on chemical kits and disposable plastic parts like sample plates and pipettes that only they sell, much like branded printer cartridges.

FILE PHOTO: RealTime Laboratories testing samples for the coronavirus disease (COVID-19) in Carrollton, Texas. – Reuters/Cooper Neill
“The vendors are in an impossible situation right now where they can’t say yes to everyone,” said Geoffrey Baird, who runs the medical laboratory at the University of Washington.
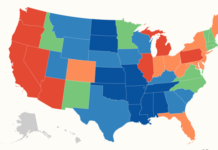
U.S. labs now run about 800,000 diagnostic tests daily, according to the COVID Tracking Project. But the United States needs 6-10 million tests per day, by various estimates.
Congress has earmarked $11 billion to support this drive, and in May, states filed plans with the government describing the equipment and supplies they would buy.
But taken together, the plans show that public health officials are not addressing the core supply-chain problem, according to the Reuters analysis.
Many states planned to buy more of these automated machines from just two manufacturers, even though the same equipment was already running below capacity or idled in other states because of shortages of chemicals or parts.

FILE PHOTO: Prism Pathology testing samples for coronavirus disease (COVID-19) in Dallas. – Reuters/Cooper Neill
Other countries, including China and Canada, have not been hamstrung to the same extent by supply shortages. Their use of less automated testing provided more flexibility in sourcing such materials.

FILE PHOTO: RealTime Laboratories testing samples for the coronavirus disease (COVID-19) in Carrollton, Texas, – Reuters/Cooper Neill
NO SIMPLE SOLUTION
Early in the pandemic, testing looked similar globally. Lab workers would extract genetic material using one instrument, and then move to a second machine to identify it. But such multi-step tests are labor-intensive and require technical expertise.
Many U.S. labs now rely on the highly automated – or “sample-to-answer” – analyzers. But some experts say this has proved inadequate because of a lack of standardized chemicals and parts.
Gary Procop, who helps lead the Cleveland Clinic’s labs, said the government could have used the Defense Production Act (DPA) to scale up multi-step tests, using existing instructions from the Centers for Disease Control and Prevention.
“That uses really standardized reagents,” Procop said of the CDC test. “You could make that in a generic form, if you will, and take the companies out of it. And then you could actually mass-produce that type of a test. But nobody’s done that.”

FILE PHOTO: RealTime Laboratories testing samples for the coronavirus disease (COVID-19) in Carrollton, Texas. – Reuters/Cooper Neill
The U.S. Department of Health and Human Services told Reuters the government had used the DPA to buy some testing supplies, but reagents used to run the CDC test are already available, so buying more would not help.
“As a result of working directly with companies to improve their supply chain, eliminate barriers, and investing through the DPA, we do expect supplies of each of these platforms to increase in the fall,” spokeswoman Mia Heck said in a statement.
Health experts also caution there is no single, simple solution to testing in a once-in-a-century pandemic that has infected more than 16 million people and killed more than 640,000 worldwide.
In China, combining patients’ samples to save supplies made it possible to test millions of Beijing residents in June, beating back a resurgent outbreak. But experts warn this method can increase false negative results and be ineffective when disease is prevalent.
Canada has built up a domestic supply chain for chemicals in multi-step tests, meaning most patients can be diagnosed within a few days. Yet this regime is more viable in a country with a fraction of the U.S. population.
“When you’re asked to process more than 1,000 samples a day – or more than 4,000 as we are now doing – you have to do some of it on sample-to-answer platforms,” said Alex Greninger, assistant director of University of Washington Medicine Clinical Virology Laboratories.
A RUN ON PANTHERS
By late April, Hologic, Cepheid, Roche and Abbott were all selling COVID-19 tests for their automated machines. Lab workers could load samples into the devices, sometimes hundreds at a time, and walk away.
Those companies became critical to the U.S. response. A May survey from the Association for Molecular Pathology (AMP) showed 47% of labs listed one of them as its primary COVID-19 testing system.
For states seeking to boost testing capacity, the most sought-after machine has been Hologic’s Panther, which can process up to 1,000 tests in 24 hours, state filings show.
“The demand has been amazing. We feel very proud of the role we’re playing,” Hologic CEO Stephen MacMillan told an investor conference in June.
The company “had virtually every governor in the U.S. just talk to us directly over the last few weeks, months, pleading their case for why they need more,” he said.
Twenty nine states and cities planned to buy a total of at least 51 Panthers, which are also used to test for HIV and other infections. Officials in Washington and North Carolina told Reuters they were still waiting on delivery.
However Hologic is not making enough COVID-19 kits to run on its existing machines – about 1,100 across the country – at capacity. At full tilt, the machines could process about 33 million tests per month, but the company makes roughly 4.8 million.
Hologic said its manufacturing teams were working around the clock while it hires more people and invests in new equipment to increase production. The company said it had already made “a huge contribution” to testing, making it possible for labs to generate more results with less hands-on time.
The runner-up in states’ plans was Cepheid, with 45 of its GeneXpert machines on wish-lists. The company, which has about 25,000 machines worldwide, is making about 2 million tests per month – enough to run two or three tests globally per machine each day.
Cepheid is focusing on customers that need rapid results, like hospitals, said Chief Medical Officer David Persing. It is working on millions of new cartridges but does not expect a dramatic supply boost until mid-2021.
‘WE WENT TO THE BUFFET’
This month, Arkansas congressional leaders warned in a letter to Vice President Mike Pence that their state’s hospitals were testing at 10% of capacity. There are shortages of key supplies from Roche, Abbott, Cepheid and Hologic, said the state’s medical director of infectious diseases Naveen Patil.
Roche told Reuters its automated equipment reduces errors, frees up staff and returns results more quickly. The company said it is increasing production capacity, and is “very intentional” about where it sends tests and instruments.
Abbott said it is expanding capacity, and closely managing supply to ensure tests get where they are needed.
Some labs have managed shortages by buying instruments from different vendors, so they can take advantage of whichever vendor’s supplies are available. But that also means they run below capacity, according to the Reuters interviews. The AMP survey found 57% of labs were running tests on at least three companies’ machines.
“It’s pretty much like we went to the buffet and got one of everything,” said University of Washington’s Baird, whose lab runs most of the state’s tests.
But as cases spiked in more than 30 states this month, some labs became overwhelmed as they struggled to get chemicals and disposable parts.
In the months ahead, separate antigen tests and gene-sequencing machines could boost capacity. The National Institutes of Health is working with companies to reach at least 6 million tests per day by December.
Some labs are also turning to suppliers of multi-step tests.
New Jersey’s RUCDR Infinite Biologics can run 50,000 samples a day in two steps. Arizona’s Sonora Quest recently announced a plan to run up to 60,000 tests a day using similar equipment.
Gary Kobinger, a Canadian researcher best known for his work on Ebola, argues that all diagnostics should be done on open platforms.
“At one point there will be a new pathogen, and the company that makes the cassette that is controlling everything is not going to be able to supply you,” he said.
“And this is where we are now, right?”
Courtesy/Source: Reuters