OCTOBER 7, 2022

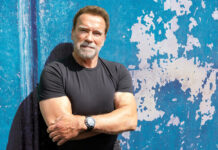
Mark Horowitz in London in August 2022. – Photo Credit: Daniel Jackont
When Mark Horowitz was 21, he began taking antidepressants.
At the time, he was feeling a “bit miserable” in school — like “a neurotic, Woody Allen kind of guy.” His medical provider suggested he start taking a selective serotonin reuptake inhibitor, or SSRI.
He never imagined the debilitating withdrawal symptoms he’d experience 13 years later while trying to come off the drug.
Horowitz recalled waking up in “animal terror,” feeling like he’d just been chased off a cliff, or enduring a “state of panic” so pervasive he took to running several miles a day until his feet bled. For the first time in his life, he thought about killing himself.
Shaken, he moved back home to Australia from London, where he’d been getting his Ph.D., to be closer to his family. His doctor prescribed a higher dose of Lexapro, the drug that he’d been taking.
Today, 19 years after he began, Horowitz is determined to stop taking his SSRI for good. He’s slowly, methodically undertaking what may be a yearslong process to wean himself off the drug, using a liquid version and decreasing his dose by just a smidgen every few weeks to avoid panic attacks.
Horowitz isn’t just any patient, though. He’s the psychiatry professor behind a major new study showing that there’s no solid link between low serotonin levels and depression.
Based on his research, Horowitz believes SSRIs like Lexapro aren’t really doing what he was once led to believe: correcting a “chemical imbalance” in his brain. In fact, he says it’s high time that this conventional wisdom is properly debunked for the general public once and for all, instead of being relegated to watercooler chatter among academics, doctors, and drugmakers.
Antidepressants were discovered by mistake

Tuberculosis patient Gloria Sydnor weighing in on a scale at Sea View Hospital, circa 1952. Previously underweight, she reached a healthy weight after participating in an MAOI drug trial at the hospital. Bettmann via Getty Images
Like Viagra, modern antidepressants were discovered by accident. In 1952, clinicians at Staten Island’s Sea View Hospital began treating tuberculosis patients with a new, experimental neurotransmitter-acting drug.
Many TB patients treated with iproniazid at Sea View likely had severe depression after months or years of hospitalization. But within weeks, they were more alert, sociable, and regaining lost weight.
These drugs were called monoamine oxidase inhibitors, or MAOIs. They prevent enzymes in the brain from breaking down key chemicals, including norepinephrine, serotonin, and dopamine.
Soon, psychiatrists began prescribing MAOIs on a larger population of depressed patients. While some of the results were promising, researchers were cautious to note that there were “varying degrees of improvement” in cases. The drug wasn’t working for everyone, and providers didn’t fully understand why.
Over the next decade or so, researchers endeavored to develop even better antidepressant drugs, with fewer undesirable side effects. During the late 1960s, scientists found evidence that the corpses of patients who died by suicide had low serotonin levels. As a result, pharmaceutical companies raced to develop antidepressant drugs targeting serotonin. The very first SSRI, Prozac, was born at Eli Lilly in the early 1970s — though it didn’t hit pharmacy shelves in the US until 1988.
Though SSRIs were chemically different from MAOIs, the thinking behind these new drugs remained largely the same. If you can make chemicals like serotonin, dopamine, and norepinephrine more available to the brain, you may be able to keep mild, moderate, and severe depression at bay.
Horowitz remembers first learning about this idea as an undergraduate. One lecture from a “top professor” really stuck with him, he said, because it laid everything out in such a clear way: Mild depression was caused by serotonin dysfunction and needed SSRIs to correct the imbalance, while more moderate cases of depression were helped by regulating both serotonin and norepinephrine. Psychotic depression, “the worst form,” was caused by dysregulation of three chemicals: serotonin, noradrenaline, and dopamine.
“I remember in that lecture thinking, ‘Wow!'” Horowitz said. “‘This is incredible, they know what’s going on.'”
We don’t know how antidepressants work
A few years after that lecture, Horowitz was a rising Ph.D. student, preparing to deliver his own first lecture on the biology and psychology of depression. But he had a hard time finding studies that showed how low serotonin levels were linked to depression.
“I’m a very meticulous, nerdy kind of guy,” he said. “I wanted to have a reference for every point I made.”
He found reviews “referencing another review” and partial findings connecting serotonin and depression, but not conclusively.
“I was so convinced that it must be there, I thought, ‘I just haven’t done a good enough search,'” he said.
Almost seven years after finishing his Ph.D., Horowitz said he still hasn’t found any compelling evidence. His latest analysis, released in the journal Molecular Psychiatry in July, is yet another review of serotonin research through the years and concludes that there is no solid link between low serotonin levels and depression.
Many mental health experts not only agree, but say Horowitz’s conclusions are nothing new.
“I was not surprised by the results of the study,” said Mimi Winsberg, a psychiatrist and the cofounder of the mental-health-treatment website Brightside, who prescribes both antidepressant drugs and talk therapy for depression. “My second reaction was, I wonder how the public will misinterpret this.”

Mimi Winsberg, the chief medical officer at Brightside Health, used to be an in-house psychiatrist at Facebook. Andy Katz
The idea that serotonin alone doesn’t control depression isn’t a shock to anyone who’s been paying attention to the field of psychiatry over the past few decades.
But after years of hearing otherwise from pharmaceutical companies on TV and general practitioners with just minutes to spare for a clinic visit and a prescription refill, it can be alarming to learn that these first-line, top-selling depression drugs — taken by upward of one in five American adults every year, according to recent estimates — don’t reliably work. The truth is that scientists still don’t really understand how they do what they do.
“There was no real evidence that serotonin deficiency caused depression,” Irving Kirsch, a psychologist and lecturer at Harvard who’s studied antidepressants and their placebo effect for many decades, told Insider.
This year, Kirsch and his colleagues conducted a review of antidepressant studies that were submitted to the US Food and Drug Administration over a nearly 40-year period. It found that only about 15% of American patients “have a substantial antidepressant effect beyond a placebo effect in clinical trials.”
Antidepressants are still widely used in large part because “no one’s found a medication that works better,” Kirsch said.
Horowitz’s paper has stirred up political and medical controversies
Horowitz’s paper has made waves in both academia and pop culture.
It is in the top 5% of the most-cited scientific articles on the internet, according to Altmetric. Fox News host Tucker Carlson has held it up on his show as evidence that SSRIs are causing more mass shootings in the US. (To be clear: They’re not. Both Horowitz and Winsberg say the accusation is not rooted in any scientific evidence.)
The more professional criticisms leveled at Horowitz’s paper tend to fall into three main camps. The first consists of mental-health experts who, like Winsberg, say this isn’t new information. We’ve known for a while that low serotonin doesn’t necessarily cause depression, and the diagnosis cannot be reduced to a simple, single biochemical root cause. But that doesn’t mean SSRIs can never work for anyone.
“Depression itself is a very complex and nuanced diagnosis,” Winsberg said. “SSRIs don’t cure people by raising their serotonin levels.” In fact, studies have shown that even artificially lowering a person’s serotonin levels does not reliably lead them into a depressed state. SSRIs are more successful for anxiety, rumination, and OCD than for “low-energy” depression cases, Winsberg said.
The second camp argues that “to dismiss the serotonin hypothesis of depression at this point is premature,” as the professor David Nutt, the head of the neuropsychopharmacology center at Imperial College London, wrote in a recent reaction to Horowitz’s paper, which was published by the Science Media Centre, a group that fights scientific misinformation.
Horowitz himself finds it “a bit funny that the experts are themselves divided,” he said. “Some are saying, ‘Of course that’s not true.’ And others are saying, ‘Of course it’s true.'”
“It seems difficult to both be utterly unsurprising and provocative at the same time,” he added.
The third camp says Horowitz and his UCL coauthor, Joanna Moncrieff, are simply too controversial to be trusted — and too keen to stir up the status quo when it comes to mental-health treatments. In 2020, the pair published a review paper, titled “Are we repeating mistakes of the past?,” on esketamine, the hallucinogenic drug that’s becoming increasingly popular for treating depression. It argued that trials of the drug did not establish efficacy and that safety concerns were underplayed.
Horowitz calls the critiques of him and his coauthor “a quite ridiculous framing,” citing leading independent experts and a UK government department, among others, who back his peer-reviewed assertions.
“In my experience, when a critic criticizes me or a coauthor personally, it means that they lack a specific argument against the points made, but do not like the conclusions reached,” he said.
Regardless of which camp his peers fall into, Horowitz said he’s concerned that the stir his paper has caused reflects the troubling way antidepressants are still being marketed to and understood by many consumers: as a simple chemical fix for what is, in reality, a very complicated, multifaceted social problem that can’t entirely be chalked up to brain chemicals.
He said he’s disappointed to see that his profession has chosen a defensive stance, instead of reflecting on what he calls the “insidious influence of drug companies” on public messaging.
“The public has been misled,” Horowitz said. “What I hope is that one of the effects of our paper is that doctors communicate more honestly and openly with patients about what the drugs may or may not be doing.”
So what are these drugs doing? The simple answer is: We don’t really know yet.
“We have some understanding, but we need to learn more,” Winsberg said. “We don’t fully understand some of the ways in which they may be alleviating symptoms.”
Are antidepressants making people numb or stimulating new brain cells?
One idea, which Winsberg backs, is that there might be some “downstream” effects of antidepressants, which is why they take several weeks to kick in. By changing the way that serotonin moves through the brain, it’s possible SSRIs “may be stimulating the birth of new brain cells,” she said. That, in turn, could have an impact on depression.
Horowitz has another theory. In studies, roughly half of patients taking antidepressants like SSRIs report a numbing or dulling of their emotions while on the drugs. If antidepressants are changing the chemistry of our brains, thereby producing changes to our thoughts and emotions, maybe they are simply blunting emotional pain.
“People become depressed because they get into difficulties in life,” Horowitz said. Maybe SSRIs work by effectively interrupting those painful thoughts.
Unfortunately, such numbing isn’t confined to negative emotions. Antidepressant drugs can also alter patients’ sex drives and increase suicidal thoughts, particularly among young people. It’s still not well-understood why that happens.
Should people stop taking SSRIs?

“The antidepressants that we now have are the least safe” depression treatments, said psychologist Irving Kirsch, a lecturer at Harvard. Tetra Images/Getty Images
Despite all the controversy about how SSRIs work and who they’re for, even Horowitz believes they can still have their uses.
“That numbing effect can be very relieving for people,” he said. “If you are in complete strife, and everything’s a panic, then being a bit numbed probably comes as great relief.”
The drugs also have short-term uses beyond treating depression, including easing hot flashes in some women going through perimenopause.
But when it comes to depression, other treatment options have been shown to do a better job.
The Royal College of Psychiatrists in the UK said in a 2019 position paper that “the routine use of antidepressants” for mild depressive symptoms “is not generally recommended,” and that more research is needed on the benefits and harms of long-term use.
In the UK, federal evidence-based guidelines suggest eight different interventions for mild depression before SSRIs are used, including guided self-help, group exercise, and meditation. For more severe cases of depression, antidepressants are recommended in tandem with therapy.
“The antidepressants that we now have are the least safe of all of these treatments,” Kirsch said of SSRIs. “You get substantially greater relapse with antidepressants than you do with physical exercise, or even with placebo.”
However, no one should abruptly stop taking their antidepressant medication, as that comes with its own set of risks, Horowitz said. The one thing everyone can agree on: Patients should talk to a knowledgeable provider first before deciding to stop, start, or taper any treatment.
For Horowitz, weaning off SSRIs has been ‘an incredible gift’

Horowitz hopes that in one or two years’ time, he can wean off Lexapro completely. Daniel Jackont
As Horowitz has slowly reduced his dose of Lexapro over time, he’s still suffered some withdrawal side effects. Overall, though, it’s been “an incredible gift” to draw down his dose “to the extent where I feel like I’m being given a second chance at life,” he said.
He expects that he may be able to come off the drug completely in a year or two. In the meantime, he’s working full time again, something he couldn’t do on larger doses, and he feels “a lot more energetic, a lot more able to think clearly.”
Even if SSRIs do fall out of favor, other drugs may soon take their place, targeting different brain chemicals. In August, a new, faster-acting antidepressant called Auvelity was approved by the US Food and Drug Administration. It’s essentially repurposed cough syrup with the addition of bupropion, an antidepressant that affects levels of norepinephrine and dopamine in the brain. Like ketamine, Auvelity acts on a glutamate theory of depression, instead of singling out serotonin.
But Horowitz isn’t sure that changing the mechanism behind a medication is as important as changing the societal conditions that lead to depression.
“I’m not sure that putting faith in some chemical to make up for social ills that tend to make us depressed is ever really going to be a successful way forward,” Horowitz said. “From what I can see, humans are mammals, and mammals have needs for community and purpose and safety. I think unless those things are being provided, there’s no drug that can solve that problem.”