MAY 17, 2020

Cows graze in a field outside of Sneedville, Tenn. on Thursday, May 14, 2020. Hancock County is the remaining county in Tennessee that has no reported cases of COVID-19. – Calvin Mattheis/News Sentinel
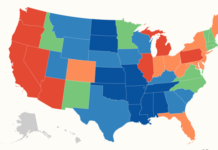
In just four months, the deadly COVID-19 virus has infiltrated every state and major U.S. city. But a scattering of remote counties continue without a single reported case, according to a USA TODAY analysis.
As of May 15, a total of 231 of 3,143 counties had no reported cases
The list is getting shorter by the day, though. In the first half of May alone, 40 counties went from zero recorded cases of the virus to at least one.
Georgia started the month with two zero-case counties. Now there are none. Tennessee also had two counties with no reported cases on May 1; two weeks later, only one remained. Iowa went from eight counties with no cases to only four by mid-May.
Counties where there are no reported cases of COVID-19*
The long stretch without coronavirus cases in some counties likely reflects an undercount from limited testing. But in others it may also reflect the benefits of being relatively cut off. USA TODAY found a strong link between population density and official infection rates across the country.
People in case-free counties said they don’t consider their communities immune, just less exposed.
“To get to Hancock County, you either have to go over a ridge or a mountain,” said Tom Harrison, the mayor of Tennessee’s last county with no recorded cases. “You don’t just drive by and see us. You have to have us on your mind to get here. And hopefully that had a little something to do with the COVID. It’s had trouble finding us.”
Counties without COVID-19
Studies have shown that the more COVID-19 tests, the more positive cases reported. USA TODAY’s analysis found states that still have counties reporting zero cases tested less of their population than others — about 30.2 tests per 1,000 residents, compared to 37.7 tests per 1,000 in states with cases in every county.
Local officials in counties without reported infections also point to another factor: The counties they live in are overwhelmingly rural, with isolated, sparse populations.
USA TODAY’s analysis included data from its own county-by-county tracking report and demographic characteristics of each county drawn from the U.S. Census and American Community Survey.
The demographic data show counties with no reported cases are mostly isolated areas, drizzled across the nation’s midsection, in the northern plains and in the Southwest.
Texas had 34 of its 254 counties reporting no positive cases – the most of any state. At least 1 in 4 counties in North Dakota, Montana and Alaska were listed as case-free through May 15.
More than 90% of such counties are rural, with a majority of residents living outside a city or large town. Most had five or fewer homes per square mile, and their populations averaged about 5,000.
Among counties with at least one case, the rate gets higher with more residents per square mile, the data show.
In counties with 10 or less people per square mile, the rate is 12 positive COVID-19 cases per 10,000 residents. In counties with more than 100 people per square mile, the case rate is nearly three times as high — 35.4 per 10,000 residents.
But researchers like Malia Jones, an assistant scientist in health geography at the University of Wisconsin-Madison, say the impact of COVID-19 can’t always be traced to an urban-rural divide.
Jones studies how infectious diseases spread. In Wisconsin, four rural counties have remained case-free, yet plenty of other rural counties have not.
“One thing to consider is, they’ve just been lucky,” Jones told the Wausau Daily Herald earlier this month. “Other rural places that are similar were unlucky, and had a case introduced early on.”
A matter of time
In Georgia’s rural Glascock County, which reported its first case earlier this month, Emergency Management Director Mike Lyons believes the county’s size may have shielded it from COVID-19 for as long as it did. Census data put Glascock County’s population at 3,009, making it the fifth-smallest statewide.
“We don’t have malls or big places to gather,” Lyons said.
Realizing Glascock County’s luck might eventually run out, county officials and first responders met for weeks to prepare before their first recorded case came.
County residents did their part – handwashing, social distancing, and complying with community mandates to close schools, nursing homes and churches – all the while, knowing that someone would eventually test positive.
“It wasn’t a matter of if it was going to happen, but when,” said Lori Boyen, chair of the Glascock County Board of Commissioners.
Glascock County got its first case May 1, when a nursing home patient at Gibson Health and Rehabilitation tested positive. The case was first reported publicly last week.
Three days later, nearby Taliaferro County, population 1,665 announced its first positive case, the last county in Georgia to do so.
Lyons said other patients and staff members at the Glascock County rehabilitation center have since tested negative.
News of the initial infections in Georgia’s last two case-free counties brought a more urgent call to action. Last week, officials began hosting drive-thru testing sites at Glascock County and Taliaferro County schools.
Lyons, the Glascock County emergency director, expects more positive cases to emerge as testing becomes more accessible.
Tennessee holdouts
At the base of verdant ridges and mountains in Tennessee, rolling pastures surround the switchback roads into Hancock County.
The drive to Sneedville, the county’s only town, is at least 40 minutes from any nearby city.
It’s a route where unrivaled natural beauty is interrupted only by a smattering of single-family homes, trailers and the scrapyards set up outside some of their doors.
Once in town, there is no Walmart, no Ruby Tuesday. There is one grocery store.
So it should come as little surprise that one of the most isolated areas in Tennessee would be the only remaining county without a case of the novel coronavirus.
Now that Tennessee’s virus-related restrictions are being lifted, things are returning to normal in the Appalachian community. But residents and businesses are still taking some precautions.
Phil Harrison, the owner of Harrison Farm & Home supply, a True Value hardware store in town, did only curbside service for five weeks, despite being considered an essential business by the state.
Now, a sign on the door asks customers to wear masks, though few are. A large makeshift plastic screen is set up at the cash register.
“We wanted to keep it down, and make sure that we did our part in keeping it from getting in here,” said Harrison, uncle of the county mayor with the same last name.
Phil Harrison believes the virus will subside some with warmer weather, but he is concerned that the town’s luck will run out as everyone resumes business as usual.
“Being secluded,” he said, “I fear that maybe we’ll get a little lax because of that.”
Per capita, Hancock County’s testing rate for the virus is nearly the worst in the state, according to an analysis by The Tennessean in Nashville. The county has administered 145 tests per 10,000 people, compared to 362 per 10,000 statewide.
But health officials said the testing disparity isn’t because of a shortage of tests in the county or people being turned away. It’s a shortage of people showing up to take them.
“It’s possible that there’s an unidentified case there, but we certainly don’t have sick people coming to the emergency room or calling our health department that can’t get tests,” said Dr. David Kirschke, medical director of the Tennessee Department of Health’s Northeast region.
Kirschke said isolation and precautions by residents seem to have made a difference. He noted that cellphone tracking data gave Hancock County residents the highest grade in the state for limiting their travel during the pandemic.
“At least relative to the rest of the state and just by that data, which has a lot of limitations, they appear to be doing well with social distancing,” Kirschke said.
Keeping it that way
Isolation has proven to be insulation in Iowa as well, as four farmland counties in the southern tier of the state still have no reported infections.
Out of 99 Iowa counties, only Adams, Decatur, Lucas and Ringgold counties remain on the zero case list – for now.
Residents and small-town businesses in Adams County are doing all they can to stay case-free.
When Iowa officials responded to the pandemic by ordering a shutdown of all dine-in food establishments across the state, folks in Corning, Iowa, population 1,400, adjusted on the fly and began offering restaurant delivery service.
Even after Iowa Gov. Kim Reynolds lifted sanctions on some counties that had fewer reported cases of the virus, Corning restaurant owners almost uniformly chose to keep their doors shut to dine-in customers, said Adams Community Chamber director Marti Gebbie.
And the owners remain defiant when it comes to serving customers in counties where cases are prevalent.
Gebbie said one restaurant manager had considered breaking rank and reopening – until the restaurant got a reservation call from a customer in West Des Moines, a city to the north in Dallas County, IA, where reported cases are among the fastest-growing in the United States.
“That’s really when they kind of were like, ‘You know what, we don’t have any cases. Do we really want people from all these other communities coming to us to dine in our restaurant?’” Gebbie said.
Even as business owners stay vigilant, Adams County Emergency Management Director Bill Lyddon has resigned himself to thinking that there will be cases in the county.
“We’re going to get some,” he said. “Whether we’ve already had some and they just haven’t been tested, or whether we’re going to get some down the line – I’m sure we will somewhere.”
While hundreds of residents in Iowa’s four remaining zero-case counties have completed assessments to see if they need to be tested, fewer than 400 had actually received tests as of last week.
Mary Williams, spokesperson for CHI Health Mercy Corning Hospital, which serves the area, believes the community is ready for a possible COVID-19 outbreak.
CHI Health, like other large health care networks, draws resources and staff from dozens of hospitals, and is able to focus those services on an area if it were in need, said Williams, who operates out of Omaha, just across the Iowa-Nebraska state line.
“We have a rather large footprint in that area,” she said. “We have the power of a system instead of one hospital, and we can go where the need is great.”
In the meantime, Williams believes residents of the four case-free Iowa counties are holding on, with daily doses of precaution and Divine intervention.
“We’re blessed,” she said. “We know things can change daily, but at this moment in time, we’re okay.”
Courtesy/Source: This article originally appeared on USA TODAY