JANUARY 24, 2021

‘African Gene Theory’ is a myth and its entrenchment in the medical community may be harming the heart health of Black men. Here’s why sodium is not to blame. – Mark Harris, Men’s Health
YOU WOULD never think that a 1988 American Heart Association (AHA) conference would set the stage for decades of debate around—of all things—sodium and race. But that’s where Clarence Grim, M.D., seeded a theory about Black health that has been difficult to uproot ever since.
Dr. Grim, then the director of the hypertension research center at the Charles R. Drew University of Medicine and Science in Los Angeles, hypothesized that high rates of hypertension among African Americans were due to the horrors of slavery, including the Middle Passage, the mass transport of slaves from West Africa to North America from roughly 1600 to 1800.
These brutal experiences forced a genetic shift, Dr. Grim argued, that allowed those who were genetically predisposed to retain more sodium in their blood (the definition of hypertension) to survive.
Descendants of the hypertensive slaves, he said, perpetuated the gene. According to headlines at the time (“Black Hypertension Theory Criticized, Doctor Says Slavery Conditions May Be Behind Problem,” read one from the Orlando Sentinel), the AHA, along with medical doctors and scientists, denounced the idea.
Dr. Grim’s theory, critics said, was based not on scientific data and evidence but on historical accounts of slavery.
Mariell Jessup, M.D., chief science and medical officer at the AHA, says that the organization recently revisited the findings. “We consulted with two internationally renowned hypertension experts who volunteer for the AHA on this issue, and both agreed that the evidence to support the Dr. Grim theory was poor. The theory was not in any way promoted by the AHA. We can find no evidence whatsoever that the slave-gene theory lives on within the AHA.”
And yet despite all this criticism, gene theory as it applies to sodium and the health of Black people settled into and persisted within certain sectors—and still rears its head.
When in 2007 Mehmet Oz, M.D., asked Oprah on The Oprah Winfrey Show, “Do you know why African Americans have high blood pressure?” Winfrey responded that Africans who survived the slave trade’s Middle Passage “were those who could hold more salt in their bodies.” Dr. Oz replied, “Perfect.”

Medical textbooks still carry information about salt-sensitivity theory—and its greater, though vaguer, cousin, gene theory.
The websites of the Centers for Disease Control and Prevention and the AHA, not to mention health websites such as WebMD and Medscape, contain references to gene theory and hypertension.
On the “High Blood Pressure and African Americans” page, the AHA states that “researchers have also found that there may be a gene that makes African Americans much more salt sensitive.”
The truth: There’s no gene.
“There is no reason to assume that major genetic discontinuities exist between different continents or ‘races,’ ” a 2004 study published in Genome Research concluded. A 2012 Harvard study found no connection between genetics and hypertension. The salt-sensitivity-gene myth persists largely because there’s a dearth of medical studies involving Black people.
It persists because it’s a systemic problem that goes well beyond sodium, one that arises via generalizations within the medical community, as well as resistance from Black people to signing on as study participants due to past mistreatment.
And it persists because it’s easier to blame genetics than it is to make big, system-wide changes to public-health policy. “We’ve been looking for this salt-retention gene for decades instead of looking at the things that we know make people sicker and die younger, like environmental injustices, like inaccessibility of health care,” says anthropologist Khiara M. Bridges, Ph.D., a professor at the UC Berkeley School of Law. “If we had preventative health care, we would have better outcomes.”
Why Salt Matters (and Doesn’t)
Black people do suffer from hypertension disproportionately. In fact, the prevalence of high blood pressure in African Americans in the United States is among the highest in the world. More than 40 percent of non-Hispanic African American men and women have the condition, and roughly 42 percent of Black men age 20 and older have high blood pressure.

Female doctor taking patient’s blood pressure – Siri Stafford
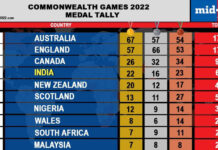
The CARDIA study published in the Journal of the American Heart Association also revealed that by age 55, 76 percent of Black people had developed high blood pressure, compared with 55 percent of white men and 40 percent of white women. Sodium intake has, for decades, been a primary target for better heart health, but that doesn’t mean sodium is inherently evil.
While sodium and salt are often used interchangeably, they are not the same thing. Sodium is a component found in salt. Salt is a mixture of sodium and chloride, with sodium constituting 40 percent of this combination.
And sodium itself isn’t a bad thing. “Sodium is an essential electrolyte that helps maintain the balance of water in and around your cells,” says Rachel M. Bond, M.D., a cardiologist at Dignity Health in Arizona.
The nutrient is necessary for muscle and organ function, as well as for maintaining stable blood-pressure levels.
That said, “excess amounts of sodium in your blood can affect the kidneys’ ability to release water and lead to higher blood pressures,” says Dr. Bond.
Hypertension can lead to heart disease, heart failure, and stroke, but scientists know now that sodium is one of many factors that may increase your risk. There’s an overemphasis placed on sodium and not as much focus on how it fits into diet, lifestyle, and family history, says Raymond Benza, M.D., the director of cardiovascular medicine at the Ohio State University Wexner Medical Center. This is particularly true as it pertains to challenges in the Black community.
“There are persistent disparities in the management of high blood pressure, including potential lack of access to care, health insurance, education, and healthy food,” says Dr. Jessup. “There is also emerging science about the impact of persistent economic stress, systemic racism, and negative health outcomes in historically marginalized populations.” So hypertension is more complex than sodium intake, and Black hypertension is far more complex than gene theory.
Yet even Dr. Benza, a funded investigator for the AHA, says that ethnic differences in sodium sensitivity have a lot to do with heredity and natural selection. “In those of African descent, the need to retain salt in the environment they operated or lived in was a necessity, because salt was a rarity in these areas. So the body built adaptations to retain salt in those climates,” he says.
The idea survives implicitly, if not always explicitly—and in order to excise it, some experts believe the medical community needs to bring a broader understanding of Black health to light.
It’s Not Just Salt
Genome mapping in the 2000s showed that there are no genetic differences among races. Perpetuating a salt-sensitivity-gene theory, many doctors argue, is racialized medical code. It’s Black health from the perspective of stereotypical conjecture and assumption rather than sound, defensible data and research.

Nurse applying vaccine on patient’s arm using face mask. – FG Trade
Sanul Corrielus, M.D., a cardiologist and the CEO of Corrielus Cardiology in Philadelphia, says that “when you have biases, you automatically jump to that voice rather than stopping, being present, and looking at the individual.”
Dr. Bond, the Arizona cardiologist, agrees that doctors and patients alike are too often willing to accept shortcut explanations based on race instead of exploring root causes. And the fact remains that the relationship between sodium and heart disease is significantly more complicated than gene theory.
The Tuskegee Study, in which doctors purposefully neglected to provide appropriate treatment to Black men in order to study the long-term effects of syphilis, lasted from 1932 to 1972 and gave Black Americans ample cause to distrust medical researchers.
“To this day it is likely why a large portion of our unrepresented minorities are going to have a fear of wanting to enroll in trials,” says Siddhartha S. Angadi, Ph.D., a cardiovascular-exercise physiologist at the University of Virginia.
In addition to an inability to access care and the possibility that Black people may not be asked to participate in studies as often as others, this distrust remains.
And low enrollment of Black study participants also has broader health ramifications. A 2018 ProPublica analysis found that the lack of Black subjects in clinical trials is limiting potential cancer treatments in African Americans.
Black participation in clinical trials for 24 of the 31 cancer drugs approved by the FDA since 2015 stands at less than 5 percent—despite non-Hispanic Black people constituting 13 percent of the U. S. population.
An Environmental Crisis
Dr. Grim, the cardiologist who presented at the 1988 AHA conference, is still consulting, researching, and writing, and he says he stands by his theory.
“It has nothing to do with race,” he says.

Father holding infant son while serving breakfast. – Thomas Barwick
“It has to do with the physiology of the individual that is salt sensitive.” He’s
a proponent of the DASH Diet, a sodium-and-potassium-conscious eating plan developed with the support of the National Institutes of Health.
“I concur that sodium and potassium are not the only cause of high blood pressure,” Dr. Grim says. “Psychological stress, economic disadvantage, living conditions, racism—these factors are known to influence blood pressure in all populations. The difference is that individuals can change exposure to excess sodium and low potassium in the diet very easily. I’ve been called a racist because they thought I was suggesting a theory based on race, but the theory is based on selective survival under unique conditions.”
Bridges, the UC Berkeley School of Law professor, says this is still faulty thinking.
“Researchers are not looking for genetic causes that might predispose white folks to death. They are just looking at Black people, which is bad science all around.” She adds that doctors wrongly assume race is a biological factor and look for data that supports that conclusion.
“Race is real not because it is a biological entity. Race is real not because there is genetic homogeneity within racial groups. Race is real because it is politically and socially real,” she says.
Gene theory and sodium-reduction prescriptions also overlook one major factor in high blood pressure: stress. “It is stressful to be a person of color and live in a racist society,” Bridges says.
Dr. Bond agrees: “Stress absolutely plays a role in our body’s ability to level out our blood-pressure readings. We, as an African American community, are more prone to a large amount of stress with systemic racism at the core, along with other social determinants of health that factor in. It’s not unreasonable for us to see why they may have higher susceptibility to higher rates of blood pressure as well.”
Then there’s the added stress of feeling that, as a Black person, with “Black genes,” you’re starting at a distinct and perhaps fated disadvantage in being able to turn your poor heart health around, says Dr. Bond, and it’s problematic to continue to just point to genetics.
“We know that in medicine we cannot just blame everything on genetics—even with heart disease,” she says. “Although important, genetics is not something we can modify.”
Courtesy/Source: This article originally appeared in the January/February 2021 issue of Men’s Health.